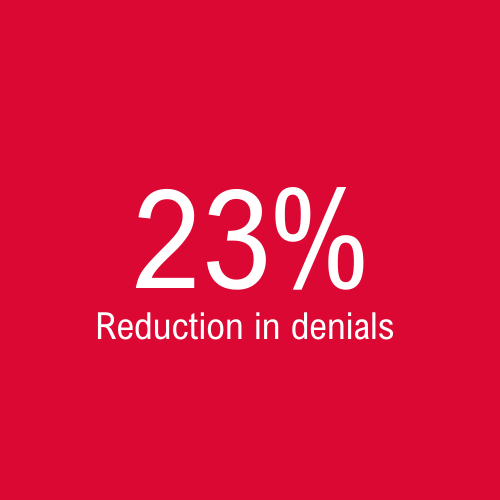
Case Study: Accurate coding of Podiatry Encounters Improves collections by 25%, reduces denials by 23%
The financial health of a healthcare practice is dependent on correct coding. Accurate medical coding improves reimbursements by reducing denials and improving clean claims submissions.
Customer Situation
Invalid Diagnosis codes can cause coding errors and inflate claim denial rates. Often, healthcare providers tend to utilize superbills and mark the nearest available codes on the superbills. One of our clients, a podiatry provider, used superbills. The providers habitually marked the 99309 procedure on the superbill and notified the billing team for processing. However, as per Medicare and Medicaid regulations, 99309 and 99252 need to be entered for the claims to get reimbursements. Due to the lack of a clear understanding of the coding guidelines, the providers marked invalid diagnosis codes on the superbill.
Challenges
Issues with Charge Entry. Lack of proper scanning of charge files led to a massive backlog on the charges.
Coding issues
Inappropriate coding resulted in higher denial rates
The Providers did not provide the right level of specificity to the diagnosis codes, which adversely impacted the clean claim submission rate
As only four-digits were marked for the CPT, the charges were kept on hold for provider assistance
Lack of information on the referring provider led to an increased number of claims getting pended
Results Summary
Solution
MBW trained a set of team members to cover the backlog and provide additional support for month-end closures
Clearing coding backlog and issues
Coding issues were all collated daily and shared with the clients via logs
Communicated day to day coding issues with our client and fixed the problem. Regular follow up was done on all items requiring clarification from providers and enter the charges on time.
Provided claim specific feedback to the providers
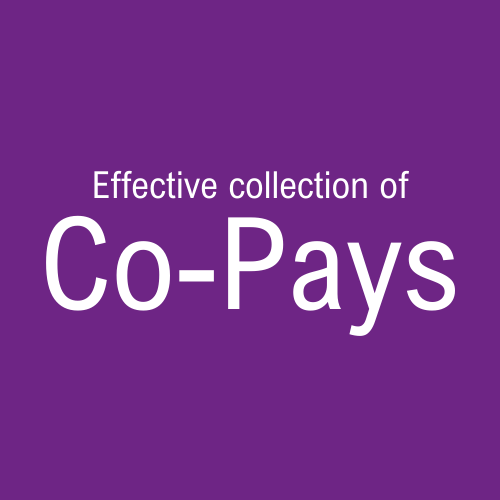
Timely Entry, Audit, and electronic filing of claims helped to improve efficiency. Eligibility Verification before entering the charges and timely follow-up with patients to capture demographic and insurance information accurately improved clean claim submission rates and, consequently, resulted in a faster turn-around of payments.
Eligibility verification at the time of service helped the practice to collect co-pays efficiently
Result
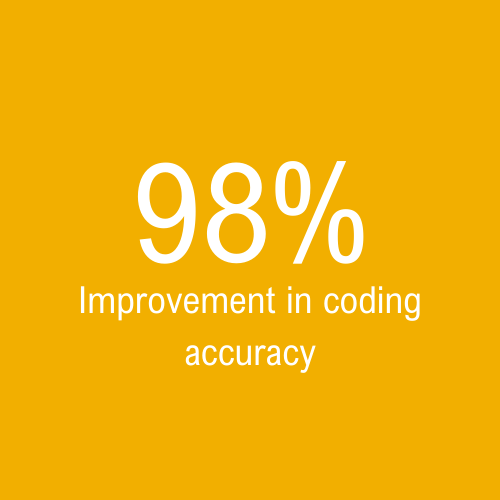
Worked with the healthcare providers to educate them on coding guidelines, and their responsibility for clinical documentation
Renewed focus on receivables management along with providers to resolve all coding and backlog issues
Improved the accuracy of medical coding to over 98%
Improved monthly collections from $33,242 in August by 25% i.e., $41,809.in December
Fixed the charge volume fluctuations and steady the charge flow
Schedule a consultation
Our focus on resolving denials by identifying and systemically eliminate the root causes, helps our clients improve revenue by a minimum of 20%. To learn about how we can help you reduce denials and improve revenue cycle metrics, please fill the form below, and we will be in touch.