Healthcare Common Procedure Coding System (HCPCS) in 2025
Healthcare Common Procedure Coding System (HCPCS) supports clean claim submission, accurate service tracking, and meeting payer-specific rules in 2025. At the present time, these codes are required for everything from outpatient procedures to Medicare reimbursements. Accordingly, knowing how to use Healthcare Common Procedure Coding System properly avoids rejections, saves time, and keeps your billing on track.
What is Healthcare Common Procedure Coding System (HCPCS)?
Healthcare Common Procedure Coding System (HCPCS) is a standardized coding system used to describe medical procedures, services, and equipment for billing purposes. It was developed by CMS to support Medicare claims and has since become a national standard across payers. You can explore must-know tips about HCPCS codes to better understand how they function across different billing scenarios. At this point, it's split into multiple levels for different use cases.
Why is HCPCS Important in Healthcare?
Without Healthcare Common Procedure Coding System, billing for non-physician services and durable equipment becomes inconsistent. Additionally, insurance payers rely on these codes to approve claims, apply coverage limits, and verify that treatment was medically necessary. As a result, accurate HCPCS use is critical for timely payment.
Difference Between HCPCS and CPT Coding Systems
While both HCPCS and CPT codes are used for billing, the key difference lies in what they represent. CPT codes describe procedures performed directly by physicians—such as surgeries, consultations, and office visits—making them ideal for clinical documentation.
In contrast, Healthcare Common Procedure Coding System (HCPCS) Level II codes cover items and services not directly performed by a physician, including medical supplies, ambulance rides, and medications. Consequently, coders often use both CPT and HCPCS codes together on a single claim to represent the full scope of services provided.
HCPCS vs CPT Codes: A Quick Comparison Guide
| Feature | CPT Codes (HCPCS Level I) | HCPCS Level II Codes |
|---|---|---|
| Governing Body | American Medical Association (AMA) | Centers for Medicare & Medicaid Services (CMS) |
| Code Format | 5-digit numeric (e.g., 99213) | 1 letter + 4 digits (e.g., A0428) |
| Scope | Physician services, outpatient procedures | Ambulance, DME, orthotics, supplies |
| Usage | Used broadly across medical specialties | Used for non-physician and ancillary services |
| Billing Type | Typically used by providers | Often used by suppliers and facilities |
| Updates | Released annually by AMA | Updated quarterly by CMS |
| Examples | 99203 (Office visit), 11721 (Nail debridement) | A0428 (Ambulance), E0110 (Crutches) |
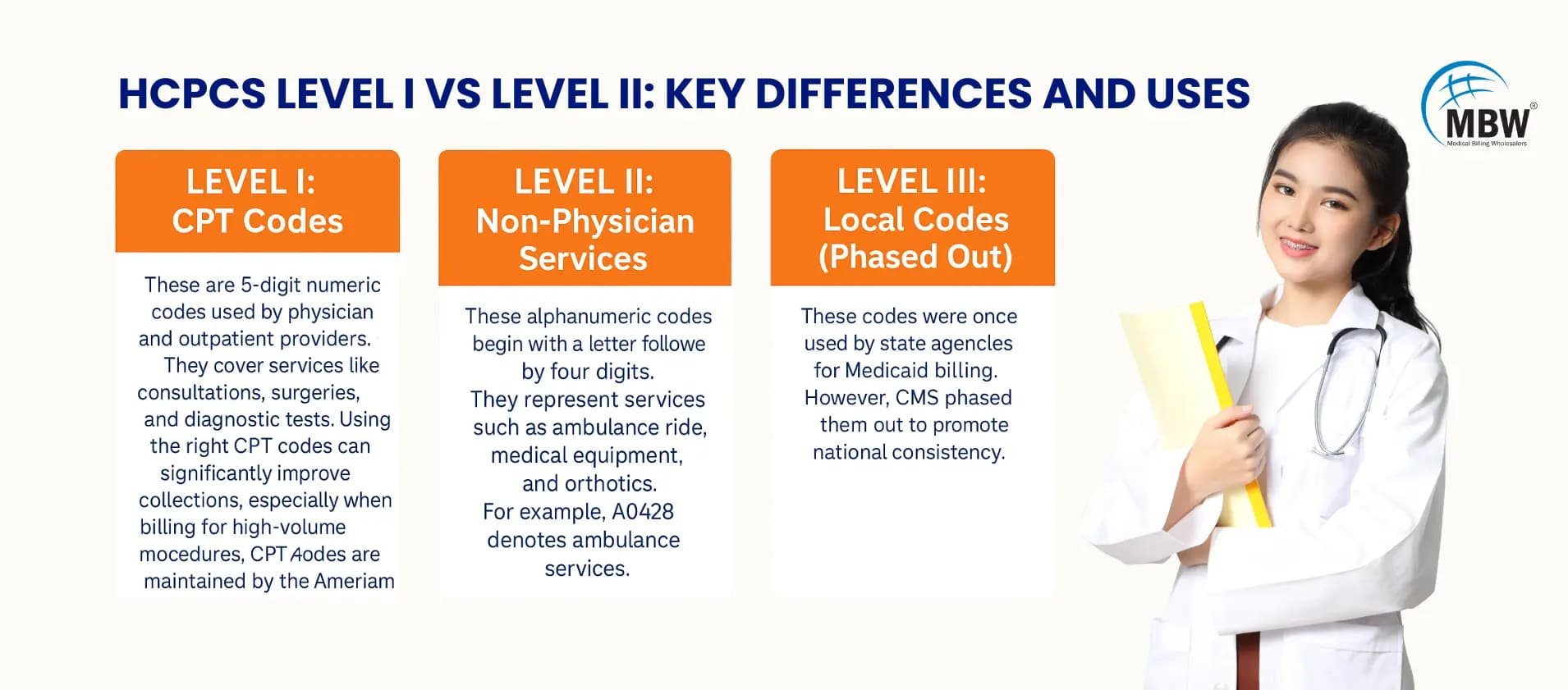
Levels of HCPCS Codes and Their Usage
The HCPCS coding system is divided into three levels, each designed for different categories of medical services and items.
Level I: CPT Codes
These are 5-digit numeric codes used by physicians and outpatient providers. They cover services like consultations, surgeries, and diagnostic tests. Using the right CPT codes can significantly improve collections, especially when billing for high-volume procedures. CPT codes are maintained by the American Medical Association (AMA).
2. Level II: Non-Physician Services
These alphanumeric codes begin with a letter followed by four digits. They represent services such as ambulance rides, medical equipment, and orthotics. For example, A0428 denotes ambulance services.
Level III: Local Codes (Phased Out)
These codes were once used by state agencies for Medicaid billing. However, CMS phased them out to promote national consistency.
What Are the New HCPCS Codes for 2025?
Each year, CMS releases updates to reflect clinical advancements and billing changes. In 2025, new codes were added, others revised or deleted. A detailed 2025 HCPCS code update is available to help providers stay aligned with correct coding practices
2025 HCPCS Code Updates: Quick Comparison
| Code | Description | Action |
|---|---|---|
| A4314 | Urological bladder insert tray | Added |
| E2102 | Artificial pancreas system | Revised |
| A0425 | Ground mileage, per statute mile | Deleted |
These changes impact billing for Medicare, Medicaid, and most commercial plans.
Why HCPCS Codes Are Critical in Outpatient Billing
Outpatient care providers rely heavily on Healthcare Common Procedure Coding System Level II codes for reimbursable supplies, transportation, and auxiliary services. As a matter of fact, many procedures performed outside of physician offices require bundled HCPCS and CPT codes to avoid claim denials.
"No HCPCS? That’s like billing with a blank check!"
Most Frequently Used HCPCS Codes in 2025
Providers searching for the most used HCPCS codes in 2025 will often encounter codes like A0428 (ambulance transport), G0008 (flu vaccine), and J1100 (injectable medications). These codes appear frequently in outpatient and Medicare claims because they represent essential services not included in CPT. For coders, referencing these high-volume codes helps reduce errors, improve billing accuracy, and support faster reimbursements.
Below is a quick-reference list of widely used codes in outpatient billing.
Top HCPCS Codes in 2025:
| HCPCS Code | Description |
|---|---|
| A0428 | Ambulance service, BLS, non-emergency |
| G0008 | Admin influenza virus vaccine |
| J1100 | Injection, dexamethasone sodium phosphate |
| E0110 | Crutches, underarm, wood, pair |
| Q4101 | Skin substitute, Apligraf |
| G2211 | Add-on code for complex outpatient E/M visits |
| E0143 | Walker, folding, wheeled, adjustable |
How HCPCS Impacts Medicare and Medicaid Billing
For Medicare and Medicaid,Healthcare Common Procedure Coding System Level II codes determine reimbursement rates and eligibility. According to CMS, over 40% of Medicare Part B claims in 2024 included at least one HCPCS Level II code, particularly for services like injections, ambulance transport, and DME.
Moreover, procedures such as home health visits and outpatient therapies are frequently reimbursed only when coded with precise HCPCS descriptors. Consequently, an incorrect or missing code can result in a full denial, with CMS reporting claim error rates as high as 7.6% due to miscoding in durable medical equipment claims alone.
Common Mistakes When Using HCPCS Codes
Errors in applying Healthcare Common Procedure Coding System Codes can disrupt billing cycles and delay reimbursements. Many of these mistakes stem from coding shortcuts, outdated references, or misunderstandings between HCPCS and CPT. Below are the most frequent pitfalls to watch out for.
Incorrect Code Selection for Services Rendered
Using a code that doesn’t match the actual service leads to denials. Always verify codes against official descriptions instead of relying on memory or outdated references. For more guidance, check out common medical billing denial codes and how to fix them.
Failure to Use Required Modifiers
Missing or incorrect modifiers can cause rejections. Some HCPCS codes—like ambulance services—need specific modifiers to convey complete billing information.
Using Outdated or Deleted Codes
Submitting old or retired HCPCS codes is a common cause of claim denial. CMS updates codes quarterly, so coders must stay current with official listings.
Confusing CPT Codes with HCPCS Level II
Coders often mistake Level I CPT codes for Level II HCPCS codes, especially when billing non-physician services or medical supplies, which leads to payment issues.
Incorrect Pairing with ICD-10 Codes
Even with a correct HCPCS code, pairing it with an unrelated or incorrect diagnosis can trigger claim rejections. Proper ICD-10 linkage is critical.
"Missed the right code? That’s like submitting claims on sticky notes."
Tips to Stay Updated with HCPCS Revisions
In 2025, staying updated with Healthcare Common Procedure Coding System revisions is key to avoiding billing errors and denials. Here are simple, effective ways to track quarterly code changes and maintain coding accuracy throughout the year.
Subscribe to MBW and Payer Update Alerts
Sign up for MBW and payer newsletters to receive alerts on new, deleted, or revised HCPCS codes. These updates are released quarterly and help coders stay current with changing regulations across Medicare and commercial payers.
Use the Latest HCPCS Codebooks
Always refer to the latest Healthcare Common Procedure Coding System Level II codebook each year. It includes new codes, discontinued entries, and modifier guidelines—reducing errors and helping your billing team avoid outdated information.
Attend Annual Coding Webinars and Workshops
Join webinars from AAPC, AHIMA, or CMS to learn about yearly code changes. These sessions include case studies, payer insights, and practical tips for applying new HCPCS codes correctly during claim submissions.
Review Quarterly Medicare Transmittals
Check Medicare Administrative Contractor (MAC) websites every quarter. Their transmittals outline code changes, billing guidance, and fee schedule updates relevant to Medicare claims and HCPCS usage.
Use Online Coding Tools and Forums
Platforms like Codify and SuperCoder provide real-time code updates, lookup tools, and user forums. These tools help clarify code use, modifiers, and payer-specific instructions through peer support.
Need Help? Talk to Our Billing Expert
In 2025, Healthcare Common Procedure Coding System continues to drive accurate claim submission for outpatient services, ambulance transport, and DME. Using the correct HCPCS codes—alongside CPT and ICD-10—helps prevent denials and supports faster reimbursements. Coders who stay updated and avoid common errors contribute directly to clean claim rates.
If your team needs help keeping up with code updates or wants to improve billing accuracy, our medical billing services can help at every stage. Contact us for a personalized review of your process.
Frequently Asked Questions (FAQs)
Healthcare Common Procedure Coding System describes medical services, devices, and supplies, helping payers process claims consistently and correctly.
CMS publishes updates quarterly on its official website, and codebooks are available from medical coding publishers.
Yes. CPT codes are Level I of HCPCS. Level II covers services not listed in CPT, like DME or transportation.
Common ones include A0428 (ambulance), G0008 (flu vaccine), and J1100 (injections).
Yes, most commercial payers use Healthcare Common Procedure Coding System for non-physician and ancillary services, especially those also billed to Medicare or Medicaid.
They now require full documentation of both programming and clinical evaluation—partial submissions have been denied.
Yes. Modifier 95 is for audio-video. Modifier 93 is for audio-only. Missing them is a leading cause of denials.
Monthly reviews are now being recommended to stay aligned with updates from Medicare, UnitedHealthcare, and other payers.
External Resource: Neurology Billing Trends 2025 – Becker’s Hospital Review
If neurology billing audits or increased denial rates are being struggled with, help is available from expert billing partners familiar with neurology requirements.