Case Study: Physician Education helps resolve BMI Diagnosis Claim Denials of over $37 K
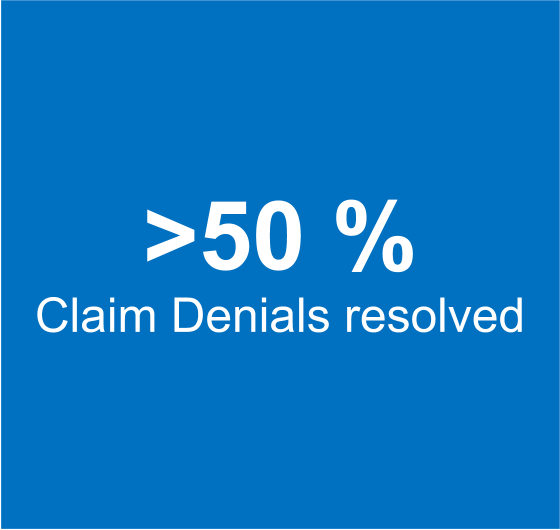
Educating the provider in submitting the Medicaid AL claims with BMI diagnosis code for specific procedures enables resolution of over 611 claims and recovery of $37 K of lost revenue.
ViewPoint
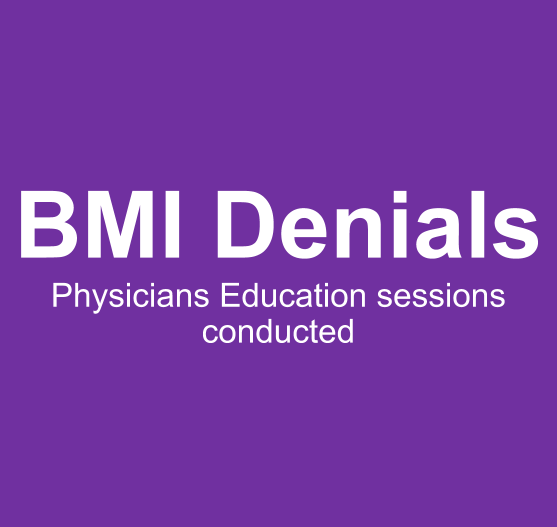
Many Primary Care Physicians lose money because of lack of understanding of payer specific claims submission guidelines. Educating physicians on their documentation responsibilities is an iterative process, that requires an understanding of the reasons for claim denials, ability to nail-down the issues that are causing the denials, determining the corrective actions, and hosting timely sessions between the denials team and the physicians to discuss them.
Results Summary
Customer Situation
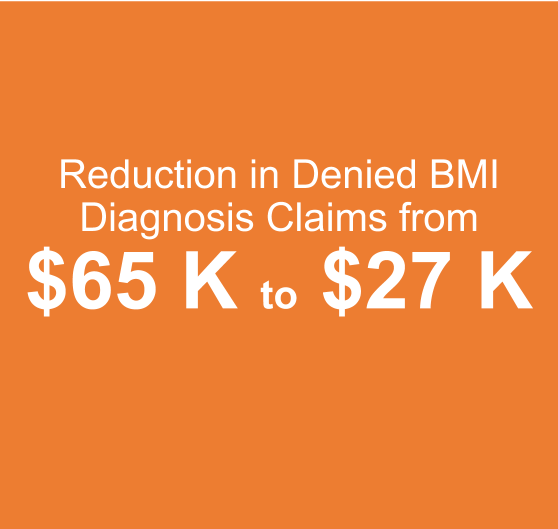
Lack of understanding of the requirement that BMI diagnosis has to be submitted along with the claim lead to a situation of 611 claims with a billed amount of $65K getting denied. This was affecting the financial health of the practice as the practice was unsure of what to do with the claims.
Challenges
Medical Billing Wholesalers was entrusted the responsibility of managing the revenue cycle for the Family practice. We encountered the following challenges.
Days in A/R were high
A huge backlog of over 1,000 unaddressed denied claims.
Solution
We took on the process of understanding the reasons for each denied claims and began understanding the trends and patterns in such denials
One of the key trends that we observed was a significant majority of claims denied Medicaid AL were denied “Procedure requires BMI diagnosis for PCP provider”
Upon further analysis we found that as per the Medicaid AL guidelines, all the primary care physicians must include a BMI diagnosis on the claim, or the claim will be denied.
We worked with the front office team of the physician and obtained the BMI diagnosis information for all the denied claims and resubmitted the claims along with BMI diagnosis.
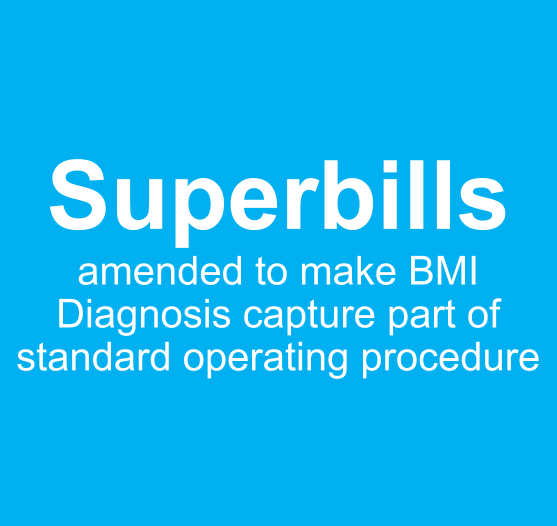
Further, we worked with the physician to make BMI diagnosis mandatory in the superbill for all Medicaid patients to avoid future denials.
Result
We were able to reduce over 50% of the AR by addressing just this issue
The claims affected to the BMI issue were resubmitted and the overall denials due to the BMI issue were reduced from $ 65 K to $ 28 K
Schedule a consultation
Our focus on resolving denials by identifying and systemically eliminate the root causes, helps our clients improve revenue by a minimum of 20%. To learn about how we can help you reduce denials and improve revenue cycle metrics, please fill the form below, and we will be in touch.