The co 97 denial code is a frustrating billing rejection that says your claim was already reimbursed under another service. As a result, many providers see revenue loss and resubmission delays due to repeat errors.
In this blog, we break down exactly what causes a 97 denial code, how to fix it, and what billing teams can do to prevent future bundling issues.
What Is CO 97 Denial Code in Medical Billing?
The co 97 denial code is issued when a billed CPT code is considered part of another service already paid. It’s also referred to as a bundled denial code or denial code 97 in payer systems.
“CO 97 is insurance’s polite way of saying: ‘Already paid. Try again never.’”
Why Does the CO 97 Denial Code Happen?
The co 97 code generally happens due to payer-specific bundling policies, improper modifier usage, or coding overlaps within a global period.
Common Causes of 97 Denial Code
| Cause | Description |
|---|---|
| Bundled procedure | Payers consider the submitted code part of another CPT already billed |
| No modifier used | Modifier 59 or 25 was missed during claim submission |
| Service in global period | CPT was billed during post-op period and not separately payable |
| Unbundled billing | Codes were split that should be submitted together |
| Duplicate claims | Same service billed more than once on the same date |
How to Fix CO 97 Denial Code Without Rebilling
Fixing the co 97 denial requires strategic coding corrections and proactive documentation.
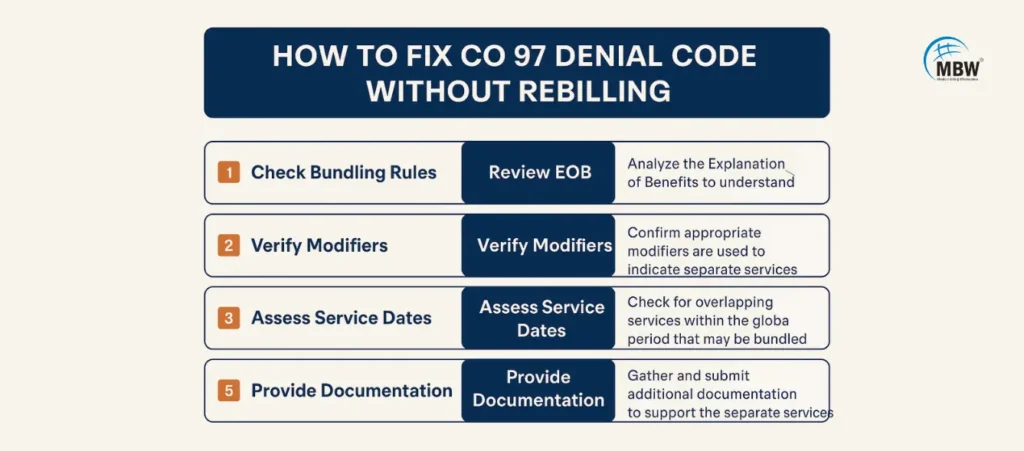
Quick Fixes for CO 97 Denial Code
| Fix | Example or Tool Used |
|---|---|
| Apply correct modifier | Modifier 25 for E/M or 59 for procedural distinctness |
| Attach supporting documents | Operative notes, separate diagnoses |
| Run NCCI edit checks | National Correct Coding Initiative bundle rules |
| Appeal with medical necessity | Clearly show service was separate and warranted |
Modifiers That Help Prevent CO 97 Denial Code
Using the right modifier can often prevent denial code co97 rejections altogether.
Modifier Table for CO 97 Denials
| Modifier | Use Case |
|---|---|
| 25 | Separately identifiable E/M during same session |
| 59 | Distinct procedural service on same date |
| 76 | Repeat service by same provider |
| 77 | Repeat service by different provider |
“Modifiers are like traffic signals for claims—ignore them, and everything crashes.”
How the Global Period Affects Denial Code 97
Billing services during the global period for 66821 or similar procedures without the correct modifier can result in a co-97 denial. Understanding when a claim falls inside or outside the surgical window helps avoid the mistake.
Bundling vs. Inclusive Denial Code: Key Differences
Although used interchangeably, bundling denial code and inclusive denial code differ in definition.
| Bundled Denial Code | Inclusive Denial Code |
|---|---|
| Denies separate billing of related services | Includes service within broader procedure |
| Can be corrected with modifiers | Often denied regardless of modifier used |
| Follows NCCI edit rules | Often plan-specific interpretations |
Related Denial Codes to Watch
When you deal with this denial code, you may also encounter related denial types like:
co-197 denial code – Previously paid claim
co119 denial code – Non-covered benefit
pi-97 denial code – Plan-specific bundling rule
denial code co119 – Unapproved service
claim denial unbundled – Over-splitting bundled services
Tips to Prevent Recurring CO 97 Denials
Preventing co 97 denial issues is possible with good practices. Here’s how:
Use claim scrubbers before submission
Verify bundling edits using payer-specific rules
Document each service’s distinct purpose
Double-check coding during the global period
Audit denials monthly for patterns
Need help managing recurring claim issues? Our Clinical Denial Management Services are designed to handle high-volume bundling and modifier rejections.
Coding Audits Can Uncover Bundling Errors
Billing audits can expose unintentional patterns behind 97 denial code errors. A well-done audit reviews modifier usage, documentation, and CPT pairings.
We recommend this detailed guide on coding compliance audits to uncover deficiencies that lead to repeated bundled denials.
Internal Education Makes a Big Difference
From understanding place of service codes to proper unbundling techniques, training your team is key. See our Place of Service Codes in Medical Coding blog to learn how coding location influences denial types.
Conclusion
The co 97 denial code can be avoided with the right mix of modifier application, documentation, and bundling logic awareness. Billers who consistently track denials and stay updated on payer rules see fewer rejections—and faster payments.
If this denial is hurting your revenue, it’s time to fix your process. Start with smarter coding, regular audits, and team training—and turn your claims into clean approvals.
FAQs on CO 97 Denial Code
1. What is the CO 97 denial code in billing?
It means the service is considered already paid under a different billed service—often due to bundling rules.
2. How do I avoid co 97 denial code errors?
Use the right modifiers (25, 59), follow bundling policies, and attach strong documentation.
3. Can CO 97 denial be appealed successfully?
Yes, if the documentation shows the service is distinct and separately billable.
4. What modifier helps prevent co 97 denial code?
Modifiers 59 and 25 are the most commonly used to avoid bundling-related denials.
5. Is co 97 denial code the same as co-197?
No—CO 97 refers to bundling. CO-197 means the service was already paid.
