Most prior authorizations for medications take between 1 to 3 business days, but complex drugs or incomplete requests may stretch the wait to 5–10 days or more.
This process often causes stress for patients and creates more work for providers. From unexpected pharmacy delays to denied insurance claims, prior authorization for medication can disrupt care. In this blog, you’ll learn what affects approval timelines, how to speed things up, and what to do when a request is denied.
What Is Prior Authorization for Medication?
Prior authorization—also referred to as pre-authorization or insurance approval—is a process in which a healthcare provider must obtain permission from the patient’s insurance company before prescribing certain medications. This step ensures the drug is medically necessary and aligns with coverage rules.
It’s typically required for:
Expensive or brand-name medications
Non-formulary drugs
Off-label use
Drugs that require step therapy
If authorization is not secured, patients may have to wait—or pay out-of-pocket.
Why Do Insurance Plans Require Prior Authorization?
Insurance companies use prior authorization to:
Review clinical appropriateness
Prevent unnecessary or high-cost prescriptions
Promote cost-effective alternatives
Ensure coverage criteria are met based on diagnosis and drug use
This process protects both the payer and the patient, but it also adds delays in treatment and a burden of paperwork for clinics.
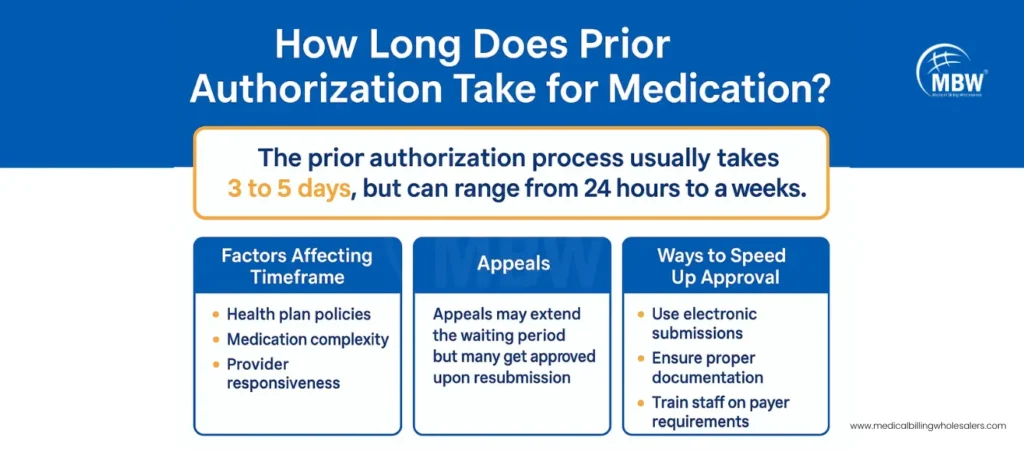
How Long Does Prior Authorization Take for Medication?
The time needed for prior authorization depends on the type of drug, payer policies, and how the request is submitted.
Average Timeline for Medication Approvals
| Type of Medication | Expected Timeframe |
|---|---|
| Formulary drugs (low-tier) | 24–72 hours |
| Specialty or biologic drugs | 5–10 business days |
| Expedited or urgent cases | Within 24 hours |
| Incomplete documentation | Adds 2–5 days extra |
So, how long does prior authorization take for medication? For most prescriptions, 1–3 business days is the average. But missing documents or payer-specific rules can extend this window.
What Causes Delays in Prior Authorization?
Some of the most common reasons for PA delays include:
Incomplete request forms
Missing documentation such as diagnosis codes or clinical notes
Use of manual fax instead of electronic submission
Submission to the wrong payer contact or department
The drug not listed on the insurer’s formulary
Each of these adds days to the wait and increases the risk of prescription abandonment.
From Days to Hours: How to Accelerate Medication Prior Authorizations
If your clinic is tired of long waits and rejections, these five strategies can reduce bottlenecks and speed up approvals:
1. Submit Requests Electronically
Electronic Prior Authorization (ePA) allows for quicker communication between your EHR system and the insurance company. It reduces errors and speeds up reviews significantly.
2. Review the Patient’s Formulary Before Prescribing
Before finalizing a prescription, check if the drug is covered under the patient’s health plan. If not, consider a generic or formulary-listed alternative.
3. Attach All Required Documentation
Payers need more than just a diagnosis—they want lab results, chart notes, previous therapy records, and clinical justification. Providing these upfront can help avoid delays.
4. Train Your Team on Insurance Rules
Each insurer has different requirements. Regular training on submission guidelines and drug-specific protocols helps prevent rework.
5. Outsource to a Prior Authorization Specialist
Partnering with a team like Medical Billing Wholesalers ensures timely submissions, consistent follow-ups, and fewer denials—letting your staff focus on care delivery.
“Even the best prescription won’t help if it’s delayed in paperwork.”
How Long Is a Prior Authorization Valid?
The validity of a prior authorization depends on the insurance provider and the medication prescribed.
| Type of Approval | Typical Validity Period |
|---|---|
| One-time use medication | 30 days |
| Maintenance medications (chronic) | 6 to 12 months |
| Refillable drugs | As outlined by the payer |
Always track expiration dates to prevent gaps in patient therapy.
What to Do If a Prior Authorization Is Denied
Denials can be discouraging—but they’re often reversible. Start by reviewing the insurer’s denial notice to understand the reason. It might be due to missing records, wrong coding, or lack of medical necessity.

If appropriate, submit a corrected request with detailed documentation, such as test results or physician notes. Some insurers allow a peer-to-peer review, enabling your provider to justify the need directly to a medical reviewer.
If approval isn’t possible, consider prescribing a similar drug on the formulary list that doesn’t require authorization. While appeals can extend the process, most succeed when supported with stronger evidence.
Why Medication Delays Due to Prior Authorization Matter
According to a AMA study:
88% of providers say PA delays negatively impact patient outcomes
24% of patients abandon their prescriptions when authorizations are delayed
34% of physicians report serious adverse events related to PA slowdowns
The impact is clear: when approvals lag, patient health is put at risk.
Final Thoughts
So, how long does prior authorization take for medication? Typically, 1 to 3 days—but that time can easily stretch to a week or more without preparation. By switching to ePA, submitting clean documentation, and staying informed about payer rules, practices can drastically reduce delays.
Better yet, outsourcing the process ensures consistent communication and faster approvals.
👉 Get in touch with our Prior Authorization Specialists and reduce your prescription delays today.
Frequently Asked Questions: Prior Authorization for Medication
1. How long does prior authorization take for medication?
Most take 1–3 business days; complex medications may take 5–10 days.
2. Why do some medications need prior authorization?
They may be expensive, non-formulary, or require step therapy approval.
3. How can I speed up the process?
Use electronic submission, provide full documentation, and check the formulary beforehand.
4. What if my request is denied?
Appeal with stronger documentation or switch to a covered alternative.
5. Who handles prior authorization in a clinic?
Often a billing or admin team—or a third-party partner like MBW.
